-
Visit Students Portal
-
Visit Lecturer Portal

On 27/6/2025, a group of Faculty of Dentistry Students helf a dental checkup at Majidi Mall Booth.

A dental check-up visit was conducted at Kurdistan Technical Institute on December 1, 2025, to promote oral health and preventive care.

On 21/10/2025, a group of Faculty of Dentistry Students visited the Kurd Genius School to perform Dental Checkups.
On 30/10/2025, a group of Faculty of Dentistry Students visited the PAP Department students to perform Dental Checkups
The Faculty of Dentistry at Qaiwan International University has a research collaboration for FYP students with the International Islamic University Malaysia (IIUM) as part of the ongoing MoU between both universities. This collaboration aims to enhance dental research, support student training, and promote academic exchange across the two universities.
Dr. Sama Naziyah, Lecturer at the Faculty of Dentistry at Qaiwan International University, will be participating as a speaker at the Research Sharing Session organized by the International Islamic University Malaysia (IIUM) with Master’s and PhD students of Dental Sciences, highlighting QIU’s commitment to advancing research and academic collaboration in the field.

As the COVID-19 pandemic continues to evolve, a growing number of individuals who have recovered from the virus report persistent, debilitating symptoms. This condition—known as long COVID—remains one of the most complex and poorly understood consequences of the pandemic.
Long COVID is characterized by symptoms that last weeks or even months after the initial infection has cleared. Recent studies suggest that approximately 10% of people infected with COVID-19 experience long-term effects. According to research published in Nature, one theory attributes these lingering symptoms to an overactive immune response that continues even after the virus is gone. Another hypothesis suggests that remnants of the virus may persist in the body, leading to chronic inflammation and organ damage—particularly in the lungs, heart, and brain.
Common symptoms include fatigue, shortness of breath, brain fog, joint pain, and cognitive difficulties. Beyond physical health, many patients report emotional and psychological distress, such as anxiety, depression, and feelings of isolation. These challenges significantly affect quality of life and the ability to return to work or everyday activities.
While ongoing research is shedding light on the possible mechanisms behind long COVID, much remains unknown. Studies are exploring everything from genetic susceptibility to the effectiveness of emerging therapies. In the meantime, healthcare providers urge individuals to prioritize self-care, maintain regular medical follow-ups, and seek support from mental health professionals when needed.
Long COVID serves as a stark reminder that the effects of COVID-19 extend far beyond the initial infection. The condition underscores the urgent need for continued research, public awareness, and a comprehensive approach to care. Globally, medical institutions are responding by funding clinical trials, establishing specialized long COVID clinics, and fostering interdisciplinary collaborations.
“Any individual can be affected by long COVID, regardless of their age or health status,” notes Dr. Tim Spector, Professor of Genetic Epidemiology at King's College London. “It is essential that individuals experiencing ongoing symptoms seek medical attention and support.”
As the world navigates the aftermath of the pandemic, long COVID highlights the importance of continued vigilance, investment in research, and compassionate care for those who are still battling the long-term consequences of this virus.
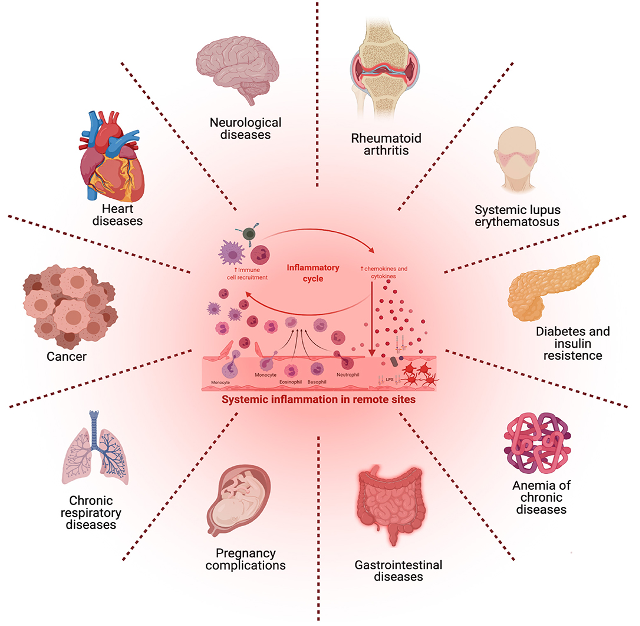
Emerging evidence suggests that periodontal inflammation may contribute to the pathogenesis and progression of various systemic conditions. Chronic periodontal infection can lead to elevated levels of inflammatory mediators, such as cytokines and acute-phase proteins, which can enter the bloodstream and influence other tissues. This systemic inflammatory response has been linked to cardiovascular diseases, including atherosclerosis and myocardial infarction, as well as diabetes mellitus, respiratory diseases like pneumonia and chronic obstructive pulmonary disease (COPD), rheumatoid arthritis, adverse pregnancy outcomes such as preterm birth and low birth weight, and even neurodegenerative conditions like Alzheimer’s disease. Conversely, systemic diseases like diabetes can impair immune function, exacerbating periodontal destruction. Understanding this bidirectional relationship underscores the importance of periodontal health in overall systemic health and highlights the need for integrated preventive and therapeutic strategies.
Various cancer types as colorectal, oral, pancreatic, lung, and gastrointestinal cancers have consistent associations with periodontal disease. On the other hand, hematological, breast and prostate cancers show associations with periodontal disease, but these links are less pronounced.
Further, periodontitis was associated with an increased risk of erectile dysfunction ED, and female infertility. In a brief, Periodontitis is linked to systemic conditions like cardiovascular disease, diabetes, and rheumatoid arthritis through chronic inflammation and bacterial spread. A key player, Porphyromonas gingivalis, disrupts immune responses, promotes systemic inflammation, and contributes to disease mechanisms via virulence factors such as gingipains. Evidence shows P. gingivalis in atherosclerotic plaques, worsened glycemic control in diabetes, and its role in autoantibody production in rheumatoid arthritis. Maintaining periodontal health is crucial for overall systemic health.